Abstract
Introduction: Myelodysplastic syndrome (MDS) is a heterogeneous group of myeloid malignant disorders characterized by defects in hematopoietic progenitor differentiation and propensity for acute myelogenous leukemia (AML). Detectable DNMT3A, TET2, and ASXL1 mutations are not only associated with increased malignant conversion risk, but also with broad Cardiovascular (CV) risk. Indeed, clonal hematopoiesis of indetetermined potential (CHIP), is associated with parametric erythroid modifications (i.e., red cell distribution width [RDW] and mean corpuscular volume [MCV]) that occurs years before hematologic malignancy development, and correlates with current patient (pt) risk for CV disease. In this study, we seek to examine the predictive value of MCV in MDS pt diagnosed with and without CV disease.
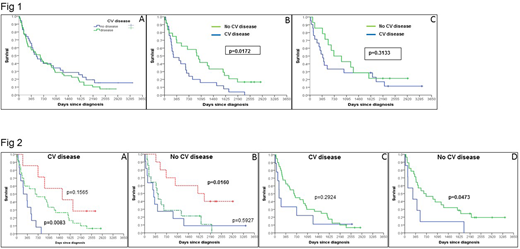
Methods: After IRB approval, 84 pt diagnosed with low-risk MDS (LR-MDS) were included for analysis. Median MCV was estimated in all LR-MDS patients to: (1) Examine overall survival (OS) in LR-MDS with and without CV disease; and (2) Detect differential OS in LR-MDS pt with and without CV disease according to baseline predictors such as hemoglobin, platelet count, RDW, platelet count, absolute neutrophil count (ANC), blast count, WHO classification and ferritin. CV was defined as the presence of one or combination of: (a) atherosclerotic hear disease demonstrated by cardiac catheterization; (2) Congestive Heart Failure (CHF); and (3) Peripheral Vascular Disease (PVD). Kaplan-Meier method was used to estimate overall survival (OS). Linear regression model was performed to adjust for multiple variable with potential impact on survival.
Results: 44/84 (52.3%) and 40/84 (47.6%) pt were CV positive (pos) and CV negative (neg). Median age for CV disease (pos) and CV (neg) pt was 72 y (range 53-88) and 76 y (range 55-91), respectively, p=0.05. In LR-MDS pt with and without CV disease, median baseline hemoglobin (Hb), RDW, MCV, ferritin and blast count were not statistically different (p>0.05 for all groups). However, baseline ANC and platelet count were 2.1 K/uL vs 1.3 K/uL (p=0.01) and 109 K/uL vs 79 K/uL (p=0.01). Median MCV for all LR-MDS pt was 99 fL. Survival in LR-MDS CV (pos) pt with median MCV > or < 99 fL was 238 vs 634 d, respectively, p= 0.01 (HR 0.6114 95% CI 0.3486 to 1.073). LR-MDS CV (neg) had survival of 831 d vs 382 d (p= 0.3). In LR-MDS CV (pos), Hb at baseline was able to segregate 3 groups with differential survival 290, 659 and 1556 d, respectively, (Hb <8 v 8-10 p= 0.008, 8-10 vs >10, p=0.1). However, different from CV (pos), hemoglobin segregated 3 distinct survival groups in CV (neg) 301, 430, 1877 d (Hb <8 v 8-10 p=0.59 8-10 vs >10 p= 0.01). RDW as a continuous measure was not predictive for all patients (p=0.085), not for CV (pos) (p=0.908) but predictive for CV (neg) (p=0.012). R-IPSS was significant in all patients (p<0.001), CV (neg) (p=0.001) but not in CV (pos) (p=0.064). Ferritin was not significant as a continuous predictor for all patients (p= 0.096) and for CV (pos) patients (p= 0.234) but was significant for CV (neg) pt (p= 0.030). WHO classification was significant in all patients (p=0.013), CV (pos) (p=0.028) but not in CV neg pt (p= 0.2).
Conclusion: CV disease is well accepted predictor of poor survival among MDS pt. However, to our knowledge, previous studies examining predictors for outcome in LR-MDS pt diagnosed with CV has not been reported before. MCV is known erythroid parameter frequently abnormal in pt with MDS. Strong correlation between TET2, deregulated IL-1 beta and macrocytosis has been recently uncovered. In our studied population, median MCV specifically discriminated different survival in LR-MDS pt diagnosed with CV disease. Notably, Hb, RDW, platelet count, ferritin and WHO classification reproduced "unique" survival among LR-MDS pt with and without CV disease. Large studies are needed. However, this report emphasizes the need for differential management in LR-MDS CV (pos) vs CV (neg) pt.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.